WA continues to manage the impacts of COVID-19, with some public health and social measures remaining in place. Western Australians are encouraged to continue to take personal responsibility and stay home when unwell, keep up healthy hygiene habits like hand washing, and wear a mask where required or appropriate. COVID-19 vaccination remains an important measure to keep the community safe and healthy.
With COVID-19 still in the community it remains important to keep abreast of any relevant announcements or updates to public health advice.
Listed below is a range of resources and links to key information sources that may be of use. Please note this page is no longer regularly updated. All efforts were made to ensure the information is true and correct at the date of publication, changes in circumstances after the time of publication may impact the accuracy of the information.
As the peak body representing women’s specialist domestic and family violence, community-based women’s health and sexual assault services in WA, we are also available to help with specific COVID-19 related queries. You can contact us at admin@cwsw.org.au.

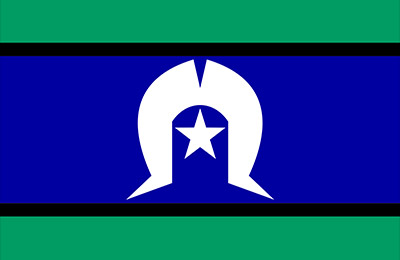
The Centre for Women’s Safety and Wellbeing acknowledges Aboriginal and Torres Strait Islander peoples as the Traditional Custodians and first peoples of Australia. We recognise the impacts of colonisation and dispossession and the contemporary disadvantage experienced by Aboriginal and Torres Strait Islander peoples. The Centre for Women’s Safety and Wellbeing is committed to working alongside Aboriginal and Torres Strait Islander women and men to end violence against their women and children in Western Australia.
The Centre for Women’s Safety and Wellbeing acknowledges the strength and resilience of adults, children and young people who have experienced family and domestic violence. We pay respects to those who did not survive and acknowledge the families, friends and communities who have lost loved ones to this preventable and widespread issue. We are committed to ensuring responses to family and domestic violence are informed by lived experience.
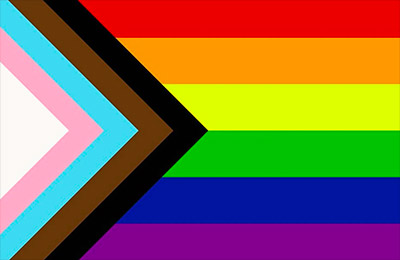
The Centre for Women’s Safety and Wellbeing recognises, welcomes and respects people of diverse gender, sex and sexuality. We are committed to greater inclusion of lesbian, gay, bisexual, transgender, intersex and queer people (LGBTIQ).

Use the quick exit button on the top right, or:
On a mac, press ⌘ and W together
On a windows, press Ctrl and W together
To remove all traces of you visiting this website, please clear your browser history.
To learn how to clear your browser history, please click here.